Technology, artificial intelligence (AI) and the Internet of Things (IoT) offer new opportunities for insurance companies to be more cost-effective and innovative. However, in order to maximize these opportunities, it’s essential that insurers not straddle two business models for too long. One model centers on legacy processes and is heavy on administrative activities and work. The emerging one utilizes technology to predict, sense, model and administer services with increasing levels of connected data.
Executive Summary
The enablers of work automation—RPA, cognitive automation and social robotics—are changing the work activities of claims professionals and agents working with carriers that have implemented them. Here, WTW's Tracey Malcolm provides a glimpse at some of the changes and describes a new metric for examining the value of improved work performance, which may help carriers pinpoint activities where AI can play a role.The enablers of work automation may be considered in three ways: robotic process automation (RPA) that covers routine tasks; cognitive automation (think AlphaGo’s recent success in winning the Go match over Lee Sedol); and social robotics, where routine and collaborative physical tasks have both robots and human capital working side by side.
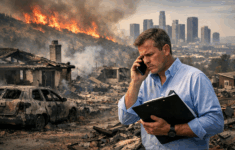
Let’s consider claim management and innovative customer service as examples of how work, talent and jobs are changing in insurance with these enablers.
In the area of claim processing transactions, Xchanging implemented RPA to improve the back office and the efficiency of processing transactions, resulting in reduced costs in claim management. (See “Robotic Process Automation at Xchanging,” L. Willcocks, M. Lacity and A. Craig; Paper 15/03, June 2015.)